Healthy Choices, Healthy Brains
By Barbara Goll, Community Education Liaison and Nutritionist
For most of us, Alzheimer’s disease is not a topic we like to think about or discuss. We fear the word and diagnosis when we hear it. This doesn’t have to be our perception of the illness. June is Alzheimer’s disease and Brain Awareness Month. It’s perfect time to better understand how eating for a healthy life impacts brain health. Eating for your brain will help you achieve peak performance in every part of your life.
Most individuals worry they have Alzheimer’s disease the moment they notice problems with their memory. Like any disease, cognitive impairment develops over years, with lifestyle choices directly impacting our brain. Our brain becomes a product of what we eat, how we move and manage stress, our quality of sleep, social connections and how we challenge our memory.
According to 2020 statistics, eight million people are living with Alzheimer’s disease. One in ten people age 65 and over have Alzheimer’s disease, and it is the sixth leading cause of death in the US. There is currently no cure for this progressive disease, and medications approved by the FDA do not slow down the disease but only offer some temporary help with symptoms.
Scientists believe lifestyle changes and nutritional therapy offer the best hope to decrease the risk for Alzheimer’s and many other chronic diseases. Lifestyle changes, known as functional medicine, delve into the root causes of health problems instead of offering prescriptions to mask the systems.
The brain is home to some of the hungriest cells in our body and uses approximately 20 percent (420) of the calories we consume daily. One reason we are both undernourished and overfed is our consumption of the wrong foods for fuel. As Americans, our standard diet puts us in a constant state of inflammation leading to cell dysfunction, destruction, and ultimately disease.
The good news is you can reverse this course at any age and with any diagnosis to sharpen brain function and avoid memory loss. Key to the change is the consumption of nutrient-dense food.
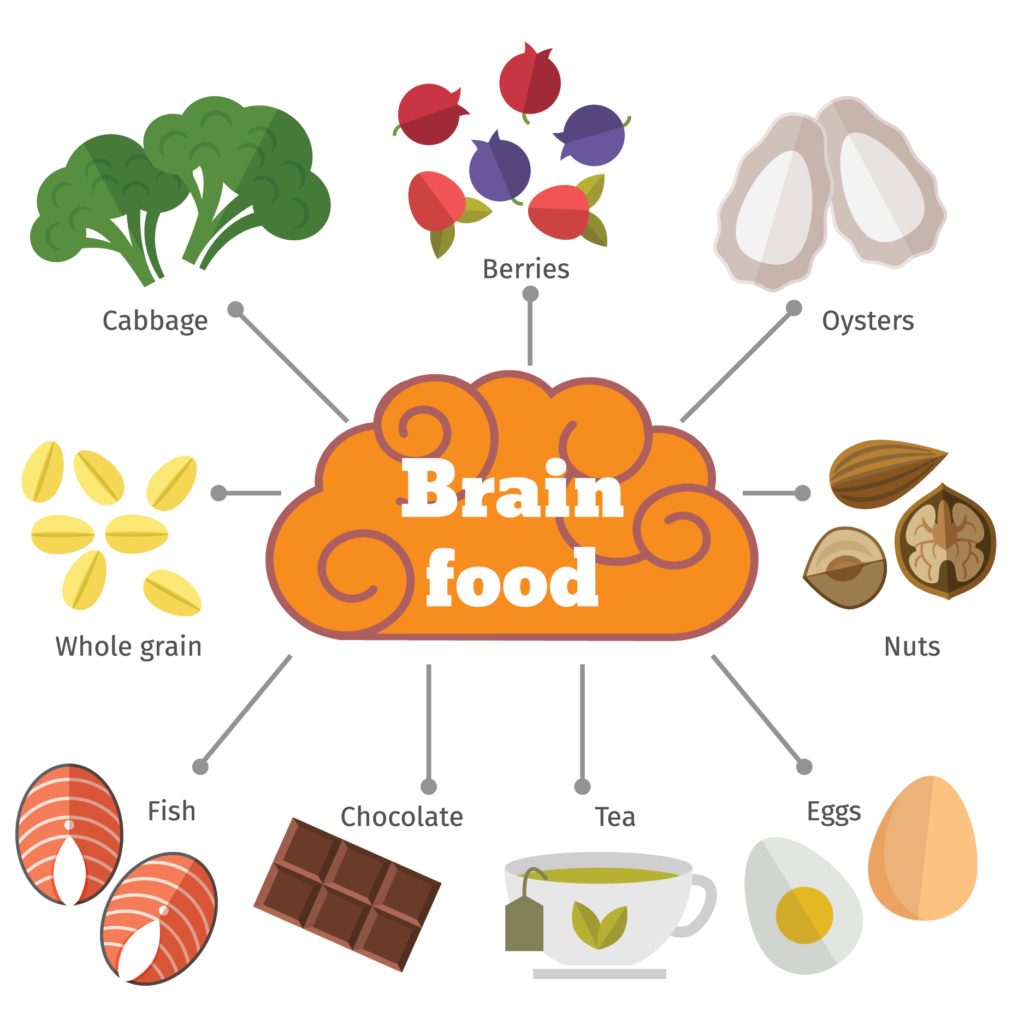
These foods include:
- Deep green leafy vegetables – at least 1 cup/day
- Rainbow colored vegetables – at least 3 cups per day
- Seafood – (2) 5 ounce servings/week (wild caught, cold water)
- Healthy oils – extra virgin olive, avocado and nut oils (first cold pressing on label)
- Nuts – 1 to 2 ounces daily (peanuts not included)
- Avocados – ½ per day
- Beans – ½ cup per day (black, navy, pinto, kidney, cannellini)
- Berries – ½ to 1 cup per day (blueberries, raspberries, blackberries, strawberries)
- Dark chocolate/cocoa powder – at least 70% cocoa on label, 1 ounce or 2 Tbs. per day
- Herbs and spices – fresh or dried
- Red wine – (1-2) 5-ounce glasses per day
It is important to note the brain damaging foods you should avoid.
These foods include:
- Saturated fats
- Trans fat
- Sugar and refined carbohydrates
- Processed foods
Bon appétit!
Barbara Goll, Community Liaison Educator and Nutritionist for Homeland at Home, offers group presentation on brain nutrition as well as many other topics on aging well, end of life decisions, as well as providing a broad overview of our Hospice, HomeHealth and HomeCare services.
To learn more, contact Barbara by emailing or call 717-221-7890.


 “There are good things happening in this world,” Laurie says. “Sending cards to patients is a great way to lift their spirits while also enabling people to take part in a positive activity during a difficult time.”
“There are good things happening in this world,” Laurie says. “Sending cards to patients is a great way to lift their spirits while also enabling people to take part in a positive activity during a difficult time.” In the United States, nearly 68 million people have hypertension, which is commonly called high blood pressure. If not treated, high blood pressure can lead to heart disease, stroke, congestive heart failure and kidney disease. With one in three people impacted by this disease, understanding its causes and treatment is critical to personal wellness.
In the United States, nearly 68 million people have hypertension, which is commonly called high blood pressure. If not treated, high blood pressure can lead to heart disease, stroke, congestive heart failure and kidney disease. With one in three people impacted by this disease, understanding its causes and treatment is critical to personal wellness. Homeland also offers telehealth. Patients are educated to take their own vitals to include their weight, blood pressure, heart rate and oxygen levels in their blood using a pulse oximeter. The information is transmitted to Homeland for daily review. This step provides current information about a patient’s wellness in-between visits.
Homeland also offers telehealth. Patients are educated to take their own vitals to include their weight, blood pressure, heart rate and oxygen levels in their blood using a pulse oximeter. The information is transmitted to Homeland for daily review. This step provides current information about a patient’s wellness in-between visits. We all need human connections, especially during the journey of grief. A smile or caring embrace from individuals in our support network can provide us courage to share our most intimate feelings of loss, and give us the strength to believe in a better tomorrow. The impact of social distancing because of COVID-19 has compounded the grieving process for individuals and families.
We all need human connections, especially during the journey of grief. A smile or caring embrace from individuals in our support network can provide us courage to share our most intimate feelings of loss, and give us the strength to believe in a better tomorrow. The impact of social distancing because of COVID-19 has compounded the grieving process for individuals and families. “I’m grateful to Brian Medkeff-Rose and Noelle Valentine, Homeland Hospice’s bereavement counselors,” says Mary Peters, MSW, LSW, Assistant Director of Social Services at Homeland Hospice. “They immediately adapted to phone sessions to offer support and guidance to all of our clients.”
“I’m grateful to Brian Medkeff-Rose and Noelle Valentine, Homeland Hospice’s bereavement counselors,” says Mary Peters, MSW, LSW, Assistant Director of Social Services at Homeland Hospice. “They immediately adapted to phone sessions to offer support and guidance to all of our clients.” The last Monday in May is recognized as Memorial Day, a special time to remember soldiers lost in wars and conflicts. Small towns hold parades and families come together for picnics. As a country, the president or vice president lays a wreath at Arlington National Cemetery at the Tomb of the Unknown Solider.
The last Monday in May is recognized as Memorial Day, a special time to remember soldiers lost in wars and conflicts. Small towns hold parades and families come together for picnics. As a country, the president or vice president lays a wreath at Arlington National Cemetery at the Tomb of the Unknown Solider. Major Henry “Hank” Heim planned every detail of his funeral. Similar to the funeral of President John F. Kennedy, Hank wanted his final farewell to represent valor, honor and duty with representation from active service members. For Hank, his funeral would be a love-letter to the country he honored and served.
Major Henry “Hank” Heim planned every detail of his funeral. Similar to the funeral of President John F. Kennedy, Hank wanted his final farewell to represent valor, honor and duty with representation from active service members. For Hank, his funeral would be a love-letter to the country he honored and served.
